Germany’s healthcare system has begun a programme that aims to improve communication and decision-making by replacing faxes, phone calls and voicemails with encrypted messaging services.
The project, which is being overseen by Germany’s National Digital Health Agency, Gematik, promises a highly secure alternative to WhatsApp that will allow patients, healthcare professionals and insurance companies to coordinate medical treatment.
Initial trials have shown that the service, known as TI-Messenger, has led to significant time savings for medical staff by freeing them from making repeated phone calls to speak with colleagues who are often too busy to answer the phone.
The service also promises to provide a more reliable, auditable alternative to fax communications, which are widely used by hospitals and clinics. Germany has a population of 83 million people and 5.7 million healthcare professionals who could benefit from using TI-Messenger.
The project reached a milestone in July 2025 when, following a government mandate, all German citizens with public health insurance who use their insurers’ apps were given the option to use TI-Messenger.
Secure communications
Marie Ruddeck, product manager at Gematik, says the project aims to develop a messaging protocol for the health sector in Germany that would allow every health institution to communicate in a secure way while still retaining control of their own data.
“The goal is to give a messaging system to everyone, so everyone can communicate with each other within healthcare. To do that, we want to give every healthcare provider in Germany the opportunity to build their own messaging system,” she told Computer Weekly.
Gematik published an initial specification for TI-Messenger in 2021, based on the Matrix open network technology standard, which is gaining traction among governments in Europe as a “sovereign” alternative to messaging and collaboration software provided by US Big Tech companies.
Matrix, which describes itself as an open protocol for decentralised secure communications, is coordinated by a non-profit community interest company, the Matrix.org Foundation.
Pharmacists see benefits of messaging
A trial of TI-Messenger in Hamburg last year showed that it can lead to significant time savings in communication between pharmacists and doctors in hospitals.
One role of a pharmacist is to review the medication of patients to check whether medicines might clash with each other. The trial found that pharmacists typically made 10 phone calls a day, which could last half an hour each, to discuss medication with doctors.
“I would love to see what we develop [with TI-Messenger] and what we learn from our mistakes shared across the borders into other healthcare systems”
Marie Ruddeck, Gematik
They often had to make multiple calls before successfully making contact because doctors were too busy to answer the phone. Pharmacists using TI-Messenger found that they only had to make one call a day.
Another trial is due to start next year in Bavaria, in a university clinic, which plans to use TI-Messenger to link patients, pharmacists and doctors.
TI-Messenger comes in two versions. TI Messenger ePA became available to all German citizens with public health insurance to download from 15 July 2025.
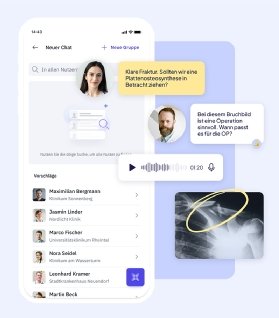
A second version, TI-Messenger Pro, also launched in 2025, intended for doctors, nurses, pharmacies and insurance companies, has yet to be widely rolled out. It allows health professionals to send secure messages, hold group chats and exchange documents.
According to Ruddeck, the majority of health insurance companies already have their own messenger service or are deploying one. Health clinics are also beginning to roll out the technology.
Take-up has been slower among doctors. Their immediate priority is to implement ePA, an electronic patient folder that became mandatory in October to store electronic patient records, which is taking precedence over TI-Messenger.
Chicken and egg
Ruddeck says one of the biggest challenges is the need to reach a critical mass of people using the TI-Messenger network so that it becomes a more useful tool.
She describes a “chicken and egg problem” where people say, “Why should I get the app to communicate with people when there are no people to communicate with?”
Ruddeck says it is important for insurers and other companies supplying TI-Messenger services to explain the benefits of messaging to the public and the healthcare industry.
“We need to persuade people to build clusters. Let’s talk with your pharmacy, your doctor, your care service,” she says.
Phillipp Kurz is the founder of Famedly, the first TI-Messenger app approved by Gematik in 2024. He suggests there should be financial incentives for doctors to use TI-Messenger and that making it easier to onboard customers would help.
Ruddeck acknowledges that it can be a challenge for large organisations to change the behaviour of staff. Clinicians may be using unofficial apps like Signal, for example.
TI-Messenger requires more work to set up than off-the-shelf messenger services, but once it’s running, it’s easy to use, she says.
Ruddeck says it was a departure for Gematik to choose to back an open source technology. “But we managed to do that because we really wanted to use this protocol. It’s state-of-the-art,” she says.
Future vision
Ruddeck says the future vision of Gematik is for an integrated healthcare system that ensures people have the right information when they need it.
Medics frequently take notes on paper – for example, when a patient is taken by ambulance to a hospital. Sometimes their handwriting is difficult to read and information can get lost. People have to spend time retyping it into computer systems.
“We want to be as digitised as possible and to have information where it needs to be, when it is needed,” she says. “We have all the information, but we don’t have the right systems yet to get it everywhere,” says Ruddeck.
“I think with TI-Messenger we can really change the behaviour away from phone calls and emails,” she adds. In the future, it may be possible to automate some answers or triage patients.
Ruddeck met with other government representatives at a Matrix conference in October and hopes to develop collaborations with other countries that are also deploying Matrix-based messenger services.
Norway, Luxembourg and the Netherlands are among the countries considering deploying the technology in their health services.
“I would love to see what we develop and what we learn from our mistakes shared across the borders into other healthcare systems,” she says.
Ultimately, it may be possible to develop a European health ID that could link patients across healthcare systems in multiple countries.




